Gestational Diabetes: Getting Diabetes during Pregnancy
Diabetes can occur during pregnancy in otherwise healthy women. This occurs due to hormonal changes and increased weight. According to the U.S. National Library of Medicine and the National Institutes of Health, three to eight of every 100 pregnant women get diabetes during their pregnancy. Gestational diabetes, also known as gestational diabetes mellitus (GDM), will go away after the baby is born, but having it increases the risk of getting type 2 diabetes in the future.
Risk Factors for Gestational Diabetes
The risk factors for getting gestational diabetes include:
- Having an immediate blood-family member with diabetes
- Being African-American, American Indian/Native American, Hispanic/Latino, Pacific Islander, or Asian American.
- Age 25 or older
- Overweight
- Previously had gestational diabetes
- Given birth to one or more babies weighing over 9 pounds
- Have pre-diabetes, impaired glucose tolerance, or impaired fasting glucose
Testing and Diagnosis
Pregnant women are routinely tested for gestational diabetes. Several types of testing are used for pregnant women. Depending upon your circumstances and risk factors, one or more diabetes tests will be administered between 24 and 28 weeks of pregnancy. A higher risk will cause the testing to be done earlier in your pregnancy.
The tests typically used to diagnose gestational diabetes are the oral glucose tolerance test, the fasting blood glucose test, and the screening glucose challenge test.
Dangers to Pregnant Women
Once diagnosed with gestational diabetes, careful health management and monitoring is required. Women with gestational diabetes are at an increased risk of high blood pressure and for needing a cesarean section delivery.
Dangers to the Unborn Baby
The mother is not exclusively at risk from gestational diabetes. The unborn baby of a woman with gestational diabetes is at risk for macrosomia (larger than normal body), hypoglycemia (blood sugar is too low), jaundice (yellowing of the skin and eye whites), Respiratory Distress Syndrome (difficulty in breathing) and low blood mineral levels.
Treatment
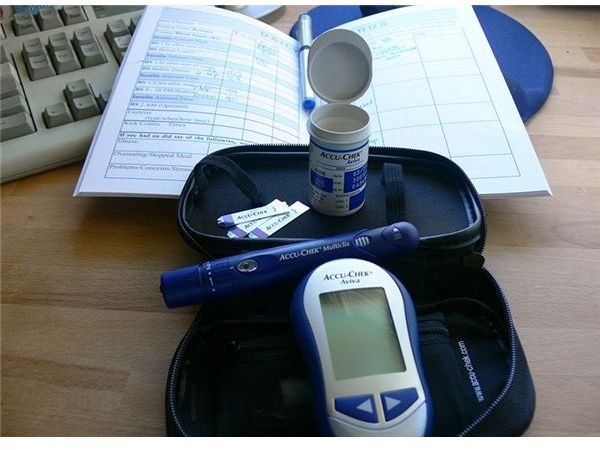
The treatment for gestational diabetes is quite similar to that of type 2 diabetes, and not that different from typical pregnancy advice – though it will require more close monitoring and adherence.
A healthy eating plan, insulin when needed, and appropriate physical activity are the main tools used to control gestational diabetes.
The End of Gestational Diabetes
Typically, within 6 to 12 weeks after delivery testing will be conducted to determine whether the gestational diabetes has cleared up or not.
Sources
Diabetes and Pregnancy. Medline Plus. U.S. National Library of Medicine and the National Institutes of Health. Last Updated: February 26, 2009. https://www.nlm.nih.gov/medlineplus/diabetesandpregnancy.html
Blood Glucose. Caroline Rhea, RN, BS, MS. [from Healthwise]. July 25, 2007. RevolutionHealth. https://www.revolutionhealth.com/conditions/diabetes/diabetes-basics/blood-glucose-tests/overview
Gestational Diabetes. National Institute of Health – Eunice Kennedy Shriver National Institute of Child Health and Human Development. Last Updated: April 29, 2008. https://www.nichd.nih.gov/health/topics/Gestational_Diabetes.cfm
What Do I Need to Know About Gestational Diabetes? National Diabetes Information Clearinghouse (NDIC). NIH Publication. April 2006. https://diabetes.niddk.nih.gov/dm/pubs/gestational/
Image Credit
Kit used by woman with gestational diabetes. Jessica Merz. Wikimedia Commons. Creative Commons Attribution 2.0 license.