Pathophysiology of Osteoarthritis: The Most Common Joint Disorder
Osteoarthritis (OA) is probably the most common type of arthritis, and is responsible for a good number of “joint pain” calls to the doctor. We shall examine the pathophysiology of osteoarthritis so we may be able to understand the function and structure of cartilage, as well as the initiating events and factors of the disease.
A Disease of Cartilage

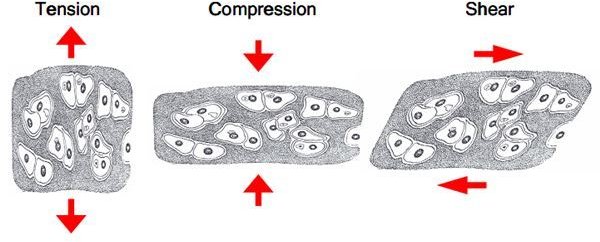
A cartilage is a tissue with compressive and viscoelastic properties which are conveyed by the extracellular matrix, which is composed largely of proteoglycans and type II collagen. Normally, this matrix goes through an active remodeling process wherein synthetic and low levels of degradation enzyme activities are kept well balanced by constant breakdown and repair, so that the cartilage’s volume is maintained.
Interleukin-1, a cytokine produced primarily by chondrocytes, stimulates the degradation synthesis that inhibits the creation of proteoglycans. Other cytokines that perform synergistically with Interleukin-1 to help matrix breakdown are interleukin-6 and tumor necrosis factor-alpha. Other enzymes that promote collagen and proteoglycan degradation are the MMPs (matrix metalloproteinases), such as stromelysin, gelatinase and collagenase. Further forms of proteinases are cathepsin, serine proteases (tissue plasminogen activator) and cysteine proteinases.
These degradative enzymes are restrained by inhibitors, which includes plasminogen activator inhibitor-7 and TIMP (tissue inhibitor if metalloproteinase). They work by developing compounds that inactivate degradative enzymes. Chondrocytes are responsible for this degradative enzyme/inhibitor balance – an imbalance will contribute to the factors resulting to OA.
Causes of Osteoarthritis
-

Aging. Wear-and-tear and normal cartilage forces are the most common cause of OA.
-
Genetics. Only recently, a gene of abnormal type II collagen has been recognized as a source of OA in a family.
-
Weight. Excess in weight has been pointed out as a factor in OA, especially in the knee and hip as four times the body weight is concentrated on these areas. One of the primary reasons for hip replacement surgery is OA.
-
Injury. This can be from previous joint trauma, the result of rheumatoid arthritis, crystal deposition, or infection within a joint. This is usually seen in younger population.
-
Post-traumatic OA. A relatively common problem, especially in athletes who sustained joint injuries when they were young and continued being active after healing. They are possible candidates to suffer traumatized joint when they get older.
Cartilage Repair

Growth factors are locally produced in cartilage; synovium contributes to the local remodeling by rousing the de novo production of proteoglycans and collagen. TGFB (transforming growth factor B) is the most potent and effective of all chondrocyte growth factors. It not only stimulates the synthesis of de novo matrix, it also works against cartilage degradation by boosting TIMP expression and interleukin-1 receptor antagonist and by reducing interleukin-1 receptor expression. Basic fibroblast growth factors and insulin-like growth factors, which are found in OA cartilage, play a role in reparative efforts; all the same, degradation ultimately outperforms restoration in OA cartilage.
Summary
To sum up this pathophysiology of osteoarthritis, MMPs and cytokines play an important role in cartilage destruction. Although the cartilage produces secretion and synthesis of inhibitors and growth factors, they appear inadequate to offset these degradative forces, which result to OA. New therapies, which focus on lessening MMP activity and increasing matrix synthesis, are now in development. Preventive measures include weight loss and proper exercise; prolotheraphy to damaged joint (increase blood supply and promote tissue repair); Glucosamin /Chondroiton sulfate (reduce long-standing pain, slow down joint narrowing, reverse cartilage damage and help joint function restoration); and Vitamin B5 supplementation.
Image Credits
- Wikimedia - https://upload.wikimedia.org/wikipedia/commons/b/ba/Osteo_of_the_hand.jpg
- Wikimedia - https://upload.wikimedia.org/wikipedia/commons/9/9e/Cartilage_forces.jpg
- Wikimedia - https://upload.wikimedia.org/wikipedia/commons/thumb/2/2f/Hip_replacement_Image_3684-PH.jpg/746px-Hip_replacement_Image_3684-PH.jpg
- Wikimedia - https://upload.wikimedia.org/wikipedia/commons/thumb/7/71/Osteoarthritis_left_knee.jpg/482px-Osteoarthritis_left_knee.jpg