Find Out More About Pseudotumor Cerebri and Foods to Eat
Overview
Pseudotumor cerebri (also known as idiopathic intracranial hypertension and benign intracranial hypertension) is caused by excessive swelling of cerebrospinal fluid in the brain. Normally, this fluid should flow naturally around the brain and through the spinal cord and back. In people suffering from pseudotumor cerebri, this fluid buildup can cause high blood pressure, vomiting, sensitivity to light, vision problems and severe migraines. Symptoms are similar to a brain tumor, but in no tumors are present in these cases. Those afflicted with this condition should learn more about PTC pseudotumor cerebri and foods to eat to help in managing this neurological disorder.
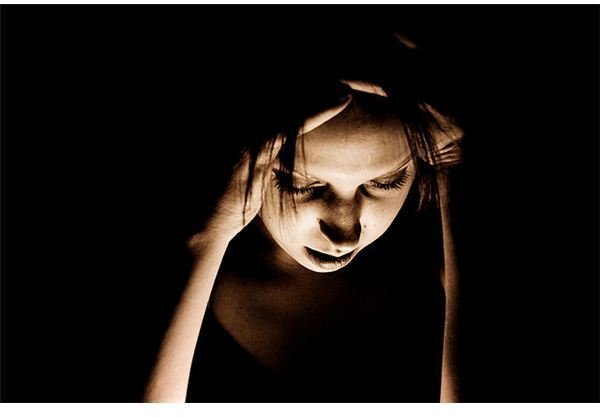
Symptoms of Pseudotumor Cerebri
Headache is the most common symptom of PTC. It is present in almost all patients, and is usually the reason why they first sought medical help. The daily headaches are normally severe, and can cause throbbing pain very different from normal headaches. These headaches will wake you up at night and keep you awake for hours.
- Nausea is also common, although vomiting is not normally present.
- Due to the headache, some patients experience pain when moving their eyes, and may feel pressure behind their eyeballs.
- Transient visual obscurations are incident wherein patients experience blurry vision for roughly 30 seconds or less, followed by a complete recovery of vision. This may involve one eye or both. An estimated three-quarters of PTC patients have experienced this symptom. Experts say that hazy vision episodes are not connected with the extent of fluid in the head or the degree of optic nerve swelling, and is not related to poor visual outcome.
- Pulse-synchronous tinnitus or pulsatile intracranial noise is common in PTC sufferers. It occurs when the patient hears a heartbeat-like, pulsating, roaring and whooshing sound.
- Visual loss is probably the most serious complication. About 5% of PTC patients experience blindness in one eye, most commonly those patients who do not return for their follow-up evaluation.
- Other symptoms include neck stiffness, numbing of the skin and joint pain.
PTC may be diagnosed by brain imaging tests, eye tests, blood tests and lumbar punctures. Treatment may include weight loss goals, lumbar punctures, medicines and surgery. With immediate treatment, serious complications of PTC may be prevented and the patient might be able to return to their usual daily activities.
Foods to Avoid
PTC sufferers can eat any food as long as it is healthy, including fruits, vegetables, fish, chicken and lean meat. They should be consumed in small, controlled portions… except for these foods:

Fatty foods** like bacon, butter, ice cream, chicken fat, meat fat, cheese, palm oil, coconut oil, beef, lamb, pork, veal, cookies, some margarines, shortening, doughnuts, chips, candies and cake.
- Salty foods like junk food, fast food, pickles, bacon, ham, salsa, cold cuts, cheese, olives, broths, anything processed and anyhting canned.
- Vitamin A rich foods like liver, beer, tomatoes, carrots, sweet potatoes and green leafy vegetables.
- Tyramine rich foods like salami, aged cheese, pepperoni, liverwurst pickled food, wine and beer.
- Caffeine. Studies show a correlation between caffeine intake and hypertension, although non-conclusive. It affects the blood flow and pressure levels but does not have an effect to the disorder directly.
Pseudotumor Cerebri and Weight Loss

Weight loss has been part of PTCs treatment for many years. As reported by Barbara Newborg, MD in 1974, nine patients all had reduction of papilledema (blurring of optic margins) when placed on a controlled and strict diet. She put them into a low calorie rice diet–an adaptation of Walter Kemper’s rice diet. Daily caloric intake was roughly 400 to 1000 calories, and included rice, vegetables, fruits and occasionally 1 to 2 ounces of meat. Daily fluids were regulated to 750 to 1250 ml, and daily sodium intake was less than 100mg. There were no reports of visual testing to see if the diet completely treated papilledema on the PTC patients.
Another report by Mark J. Kupersmith, MD, Director of the Neuro-Ophthalmology Division, and colleagues described 38 women with PTC who lost weight (around 2.5 kg) and 20 women who did not lose weight. Result of visual field deficits and visual acuity were similar; however, papilledema and visual fields improved more quickly in the group with weight loss–28 patients in 4 months compared to the group without weight loss, which resolved 8 patients in 1 year.
Johnson LN, Madsen RW, March GA Jr. and Krohel GB studied 15 PTC patients treated with acetazolamide coupled with weight loss for 6 months. Nine out of 10 patients who lost 6% of their weight had grade one progress on their papilledema, while the four who did not lose weight had no development in their papilledema grade despite taking the prescribed medicine religiously.
Weight loss is an important part of treatment and the cornerstone of PTC therapy. A low salt, low fat diet and weight reduction of 5 to 10% of overall body weight is recommended to treat this neurological disorder. Modest weight loss is more realistic and likely to succeed than the aggressive weight loss plan. Patients suffering from this condition must take pseudotumor cerebri and foods to eat seriously. Studies show that fluid and sodium restriction and losing weight in general reduce intracranial pressure in the brain.
Disclaimer
This is not medical advice and is not meant to treat, diagnose, prescribe or cure any ailment. Check with your physician first before following any advice you have read on BrightHub.com. Consult your physician before you start, stop or change anything that has been previously prescribed to you.
Image Credits
- Muffet - https://farm1.static.flickr.com/24/98277342_c746b58495_z.jpg
- SashaW - https://farm4.static.flickr.com/3291/3108464695_e375c23c46_z.jpg
- Steven Depolo - https://farm4.static.flickr.com/3476/3402657215_b453b1305f_z.jpg?zz=1
- GoodNCrazy - https://farm3.static.flickr.com/2724/4407297947_ae7a24c827_o.jpg
References
- National Institute of Neurological Disorders and Stroke - https://www.ninds.nih.gov/disorders/pseudotumorcerebri/pseudotumorcerebri.htm
- MayoClinic.com - https://www.mayoclinic.com/health/pseudotumor-cerebri/DS00851
- MedlinePlus: Trused Health Information for you - https://www.nlm.nih.gov/medlineplus/ency/article/000351.htm
Sample contents.