Supraventricular Tachycardia and Asthma
Supraventricular Tachycardia and Asthma
Supraventricular tachycardia (SVT) causes occasional episodes of a fast heartbeat, which is a heart rate greater than 100 beats per minute. A normal adults heart rate ranges between 60 and 100 beats per minute.
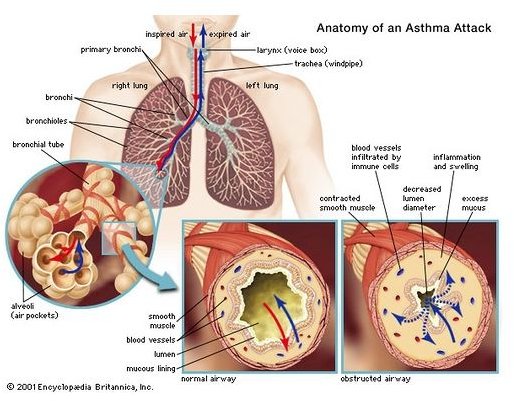
Some asthma inhalers used to treat asthma, can increase the risk of developing an episode of SVT. An episode can last seconds, minutes, hours or even longer (which is rare). Supraventricular tachycardia and asthma can sometimes be a dangerous combination, which is why it is important that medical personnel be aware if you have a history of asthma.
Possible symptoms could include a pulse rate of 100 to 200 beats per minute, palpitations, shortness of breath, chest pain, rapid respiration, an increase or decrease in blood pressure, loss of consciousness or numbness in various parts of the body.
The general protocol for an episode would be to inject Adenisone into the vein to stop an episode of supraventricular tachycardia. However, caution is recommended when administering inhaled or intravenous Adenosine in patients with asthma. Some asthmatics cannot have this drug. Adenosine is known to cause bronchoconstriction in asthmatics. Verapamil is an alternative. Verapamil is a calcium-channel blocker that relaxes the blood vessels.
A clinical trial for intravenous (IV) asthma treatment is being conducted by the National Institute of Health to see if patients going to the emergency room with an asthma attack can benefit from an IV dose of an approved drug, Montelukast sodium, which contains the same active ingredient as Singular. Montelukast is presently used as a maintenance drug for asthma and to relieve the symptoms of seasonal allergies.
Images

Click on images to enlarge.
Supraventricular Tachycardia Diagnosis
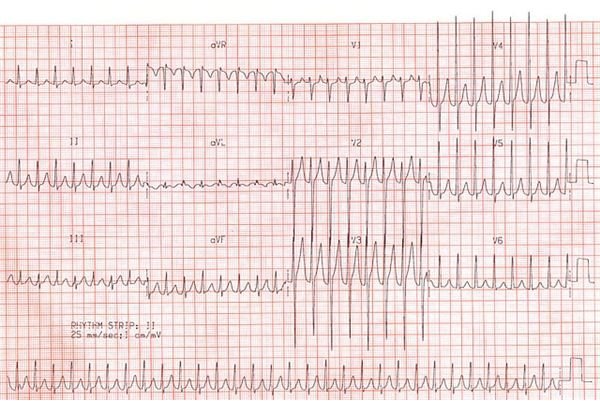
Supraventricular tachycardia is diagnosed with an electrocardiogram (EKG). If the patient is experiencing a supraventricular episode during the EKG, a clear diagnosis can be made.
A 24 hour event halter monitor can also be used to record the heart rhythm.
A loop monitor which records the hearts rhythm can be worn. The patient can press a button to record any episodes. The loop monitor records is then downloaded using a telephone.
Conclusion
The best way to control your asthma attacks would be to avoid whatever triggers your asthma attacks, which is not always possible. Allergy shots are also available, which can desensitize your system over time.
If you experience an episode of supraventricular tachycardia, always be sure to inform any medical personnel if you have a history of asthma.
Discussing with your personal physician what steps should be taken when an episode occurs is very important. Each case is different and only your personal physician is aware of your medical history and can advise what would be best for your case. Don’t be afraid to ask questions or to get a second opinion if you don’t feel comfortable.
References
National Institute of Health: https://www.ncbi.nlm.nih.gov/pubmed/15824553
The Mayo Clinic: https://www.mayoclinic.com/health/heart-arrhythmias/DS00290/DSECTION=causes
Bio-Med Respiratory Research: https://respiratory-research.com/content/7/1/139
Photos courtesy of Flickr:
https://www.flickr.com/photos/42045498@N05/4359225668/ (by Seegul)
https://www.flickr.com/photos/allmothers/4419086543/ (by allmothers)
https://www.flickr.com/photos/popfossa/3992533568/ (by Popfossa)
This post is part of the series: Asthma treatments
Asthma medications used for treatment and maintenance of asthma